Background
Heparin-induced-thrombocytopenia (HIT) is a life-threatening disorder. Clinicians caring for patients at risk are often unaware how to diagnose and manage HIT.
Methods
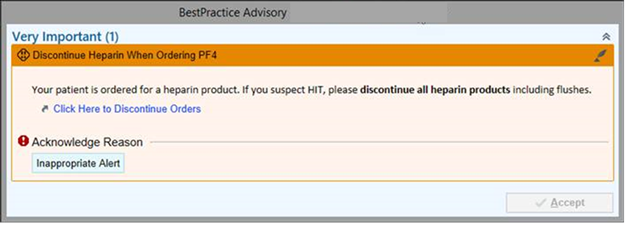
We implemented tools at Brigham and Women’s Hospital to improve management of suspected HIT cases: 1. Best Practice Advisory (BPA) encouraging heparin discontinuation when ordering Platelet Factor 4 (PF4) testing (Figure 1), 2. Questions requiring 4T calculation when ordering a PF4, 3. Randomized BPA recommending discontinuing the PF4 order if 4T score <4. Interventions were assessed in pre and post implementation time periods from 12/17/2017 to 4/24/2021. Chi-squared analysis was performed between groups.
Results
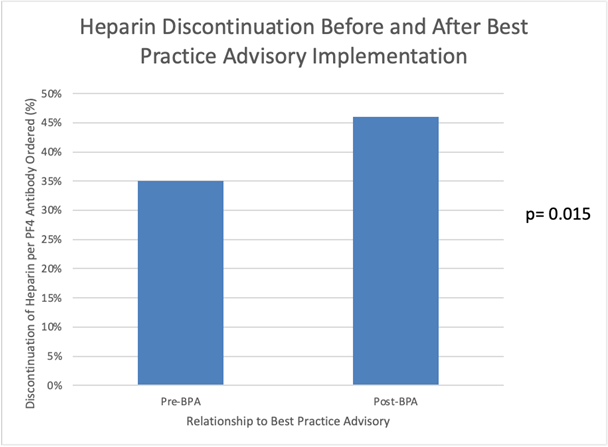
Heparin discontinuation increased from 35% to 46% (p = 0.015) after BPA implementation. In the pre-4T order questions group, 4T scores were documented in 30% (85/272) compared to 100% (547/547) in the post-4T group. In the pre-4T group, only 27% of PF4 tests were appropriate. No change in appropriate PF4 ordering was seen with the randomized BPA: 81% appropriate orders with the BPA versus 76% without (p=0.13). Subspeciality appropriate PF4 test ordering varied.
Conclusion
Implementation of electronic decision support to stop heparin in patients with suspected HIT was successful, which can decrease mortality, but improving appropriate PF4 test ordering was not affected by similar strategies.